Percutaneous distal venous arterialisation (pDVA) in a patient with no-option chronic limb threatening ischaemia (CLTI).
Keywords:
Chronic-Limb-Ischaemia, Vascular-Surgery, Surgery, Distal-Venous-ArterialisationAbstract
Introduction
This case study presents the management and follow-up of a patient with chronic limb ischaemia
(CLI). Owing to the lack of viable treatment options available, the patient elected to undergo distal
venous arterialisation (DVA) as an experimental procedure to restore perfusion to his
compromised limb.
Methods (History and Management)
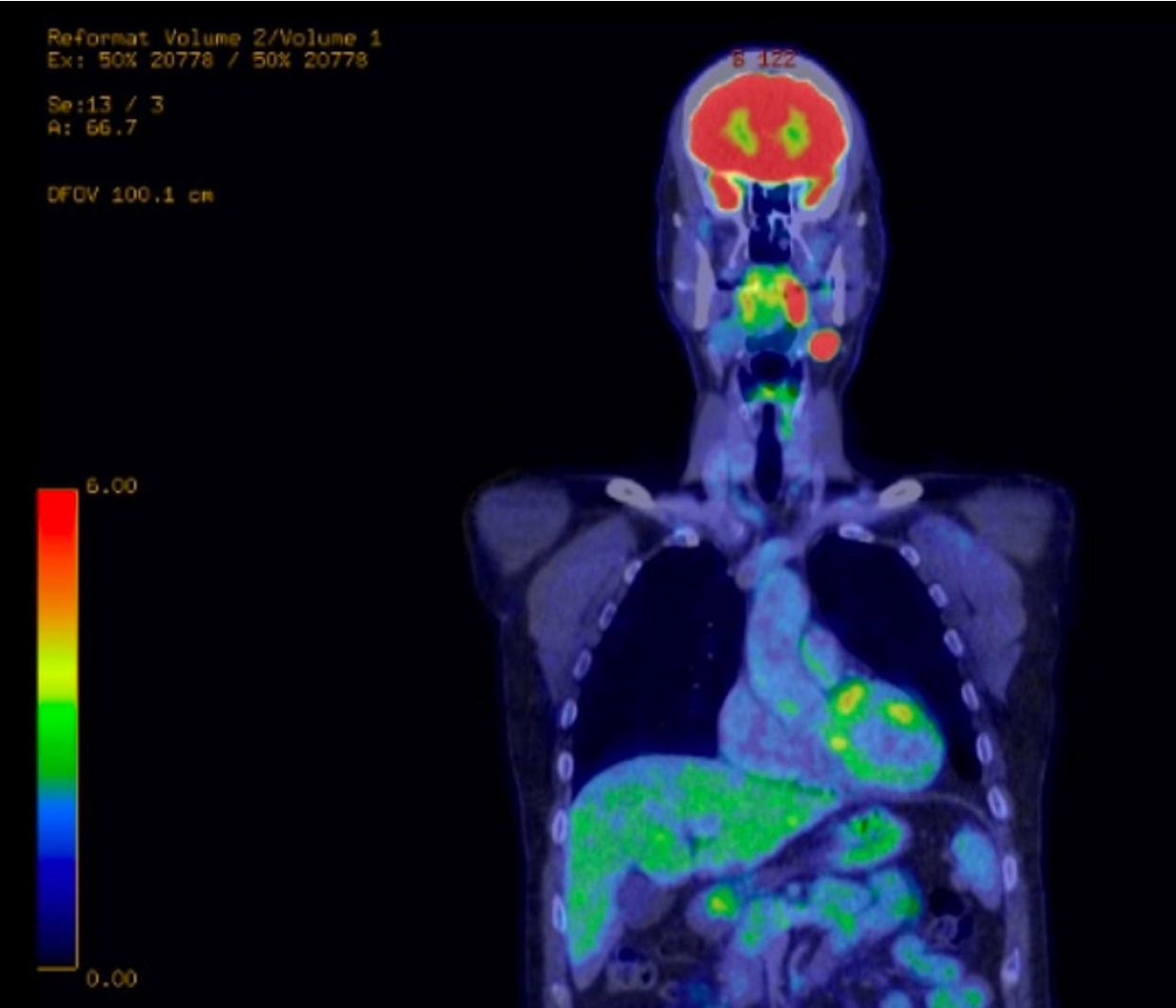
80-year-old male presenting with CLI of the left leg on a background of right below-kneeamputation, diabetes, COPD, atrial fibrillation, and antiphospholipid syndrome. Investigations
revealed distal vascular disease of the left leg, poor flow into the foot with no named arteries patent
identified on pre-treatment angiogram. Patient was consented for DVA as progressive necrosis of
the toes had occurred despite medical management with vasodilators and attempted endovascular
procedures.
A fistula tract was created endovascularly between the posterior tibial artery and vein with
covering stents placed across the fistula. Proximal valves of the vein were rendered incompetent
with balloon venoplasty. Competing collateral veins were then occluded with covered stents two
weeks post procedure due to outflow shunting identified on angiogram.
Results (Outcomes)
Angiogram identified good flow around the plantar arch post procedure. Examination two months
post-DVA showed marked improvement with granulation tissue at wounds. Midfoot was found to
be warm and perfused with good doppler signal from the arterialized vein. Healing continued at 6-
month follow up with the wound deemed fully healed 1-year post procedure.
Conclusions
DVA represents a novel procedure for patients with no-option CLI with a patent/stump tibial artery
and adjacent vein. Case based evidence suggests that using standard endovascular techniques and
equipment DVA can potentially avoid major amputation. Future studies to compare outcomes of
DVA in CLI patients vs controls will be needed to evaluate the effectiveness of endovascular DV
Published
Issue
Section
License
Copyright (c) 2023 Zachariah M Raouf, Madhurima R Chetan, Rafiuddin Patel, Tina Mackinnon, Andrew MacDonald, Andrew Wigham, Raman Uberoi, Dominic PJ Howard

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors will retain copyright alongside scholarly usage rights and JNDS will be granted publishing and distribution rights.