Ischaemia reperfusion induces the release of donor derived Passenger Leukocytes (PLs) during normothermic machine perfusion (NMP) of the liver- a new opportunity for ex situ graft leukodepletion?
DOI:
https://doi.org/10.37707/jnds.v2i4.202Abstract
Fungai Dengu1, Tamsyn Clark1,3, Hussain Abbas1, Etohan Ann Ogbemudia1, Faysal El Gilani1,
David Nasralla1, Peter Friend1, James Fildes2
1. Oxford Organ Perfusion Lab, Nuffield Department of Surgical Sciences and Oxford Biomedical Research
Centre, University of Oxford, Oxford, UK
2. The Ex-Vivo Lab, Division of Cell Matrix Biology and Regenerative Medicine, School of Biological
Sciences, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester Academic
Health Science Centre, Manchester, UK
3. Institute of Biomedical Engineering, University of Oxford, Oxford, UK
Background
Passenger Leukocytes (PLs) are implicated in both the direct and semi-direct pathways of allorecognition which is the process that underpins acute allograft rejection1. The majority of liver-derived PLs are short lived and predominantly impact early recipient immune responses2. Removal of PLs has been shown in kidney, lung and vascularised composite allografts to reduce early allograft damage and abrogate ejection3. We aimed to assess the use normothermic machine perfusion (NMP) to investigate PL kinetics and explore PL depletion strategies in donor livers.
Methods
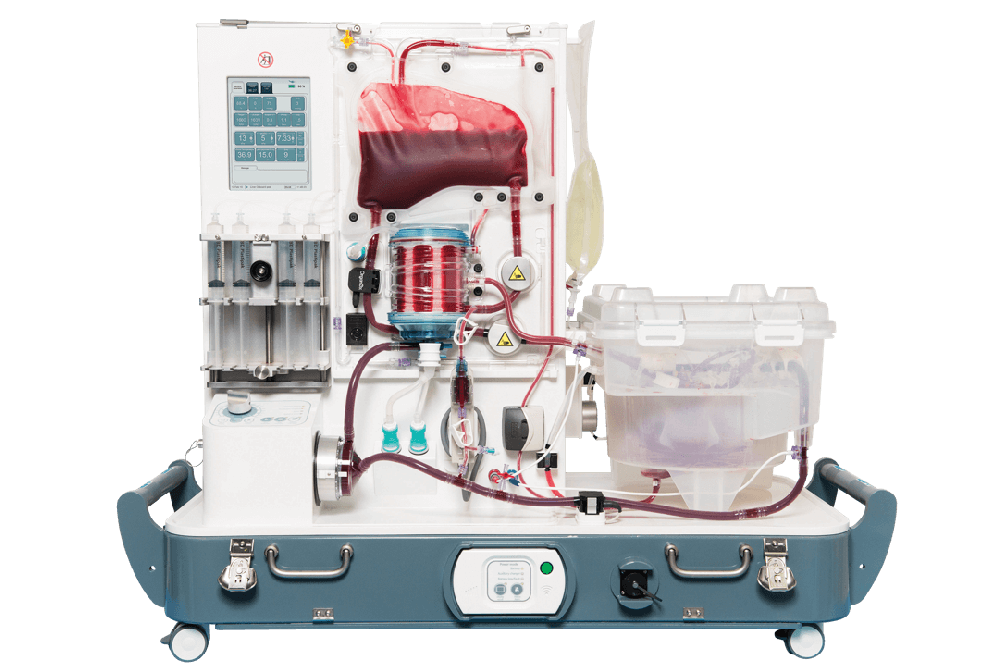
Porcine livers (N=4) procured in a donation after circulatory death (DCD) model were preserved with sequential static cold storage then NMP. During NMP, livers were subjected to repeated 20 min warm ischaemic hits (IH) followed by 30mins of NMP using a leukocyte depleted autologous RBC based perfusate. Leukocytes were quantified using the Sysmex® cell counter system and samples stored for flow cytometric analysis.
Results
In total, 3.4x106 PLs are effluxed into the circuit immediately after initiation of NMP, this falls rapidly to 1.35x106 by 30 mins. Following the first IH, a further efflux of occurs with a peak of 3.74x106 occurring. The second IH also induced an efflux of cells (1.61x106) with lymphocytes representing the predominant leukocyte sub-type in each efflux.
Discussion
During NMP, there is an inducible and reproducible efflux of graft derived PLs into the circuit that is composed of predominantly lymphocytes with unexpectedly low numbers of monocytes. Removal of these PLs from the perfusate during NMP may therefore be feasible using an in-line leukocyte-filter.
References
1. Alsughayyir, J., Motallebzadeh, R. & Pettigrew, G. J. Are donor lymphocytes a barrier to transplantation tolerance? Curr. Opin. Organ Transplant. 23, 90–96 (2018).
2. Mastoridis, S. et al. Impact of donor extracellular vesicle release on recipient cell “cross-dressing” following clinical liver and kidney transplantation. Am. J. Transplant. ajt.16123 (2020). doi:10.1111/ajt.16123
3. Stone, J. P. et al. Mechanical removal of dendritic cell–generating non-classical monocytes via ex vivo lung perfusion. J. Hear. Lung Transplant. 33, 864–869 (2014).
Published
Issue
Section
License
Authors will retain copyright alongside scholarly usage rights and JNDS will be granted publishing and distribution rights.